Prescription Coverage
Overview
State employees automatically receive prescription coverage administered by CVS Caremark when they enroll in one of the State's Anchor medical plans.
Note: This video refers to electing a Primary Care Physician (PCP) to coordinate care. While it’s always a good idea to establish a relationship with a PCP, employees (except RIBCO, RITA, non-Union State Police, non-Classified union and non-union education and college employees) who are enrolled in the Anchor plans are not required to designate a PCP to coordinate their care.
Coverage Details
Key Plan Features
- Combined out-of-pocket maximum for medical and prescription
- Anchor/Anchor Plus prescription drug co-pays levels:
- Generic: $10
- Preferred Brand-Name: $35
- Non-Preferred Brand-Name: $60
- Specialty: $100
- PrudentRx for Specialty Drugs
- This program is designed to reduce your out-of-pocket cost for certain specialty drugs. If you or a dependent takes a specialty drug on the PrudentRx drug list, you would receive the drug from an in-network pharmacy with no out-of-pocket cost.* If you choose not to participate in PrudentRx, your specialty fills will be subject to 30% coinsurance. For more detailed information on the program review the PrudentRx FAQs.
- * EXCEPTION: If you are enrolled in the Anchor Choice plan with HSA, you must fully satisfy your deductible before you are eligible to obtain your specialty drug at no out-of-pocket cost, unless you have been prescribed a medication that is qualified as “preventive care” by the IRS. You may still choose to use available manufacturer copay assistance to help cover your out-of-pocket cost before you have met your deductible, but you will not be eligible for $0 out-of-pocket cost under the program until your deductible has been satisfied.
- Anchor Choice prescription drug costs are 100% of retail cost until the deductible is met, then Anchor/Anchor Plus co-pay levels apply until the out-of-pocket maximum is met.
- EXCEPTION: Under Anchor Choice the Anchor/Anchor Plus co-pay levels are applicable for certain preventive therapy drugs before the deductible is met and until the out-of-pocket maximum is met. A broad but not completely comprehensive listing of these drugs can be found on the preventive therapy drug list below in the "Drug Lists & Costs" section.
- Savings Advisor – A new tool on Caremark.com that may help you save on the medications you need. View the Savings Advisor flyer or click on the "Drug Lists & Costs" tab for more information.
- Maintenance Choice – Save money by obtaining 90-day supplies of long-term maintenance medications for the co-pay price of a 60-day fill.
- AccordantCare™ – Provides free one-on-one support from nurses who are specially trained in complex conditions.
What You Should Know
- Coverage is administered by CVS Caremark. You can fill short-term medications at any of the 68,000 participating pharmacies nationwide (including 7,500 CVS/pharmacy locations). If you use a non-participating pharmacy, complete the CVS Caremark Rx Claim Form to receive reimbursement for your out-of-network prescription claims.
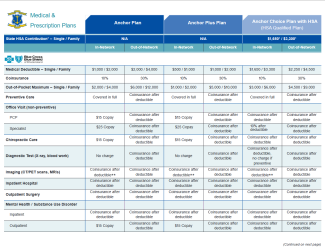
- See the Medical/Prescription Plans Comparison or contact CVS Caremark for details regarding your prescription coverage.
- If you are enrolled in the Anchor Choice Plan, you will be required to pay the full cost for your medications until you reach your annual plan deductible. After you meet the deductible, you pay only the co-pay until you reach the annual out-of-pocket maximum. However, this deductible rule does not apply if you take medications on the Preventive Therapy Drug List - you pay only the copay for these medications even if you have not yet met your deductible.
- The State plan covers a variety of preventive prescriptions and products at no cost to you and any covered dependents. See CVS Caremark® Preventive Services List for complete detail on what is covered. (Note: Your doctor must write a prescription for these preventive services to be covered by your plan, even if they are listed as over-the-counter.)
- See the CVS FAQ for answers to common questions about your prescription coverage.
Plan Comparison
Click on the chart below to see the prescription coverages under Anchor, Anchor Plus and Anchor Choice.
Coordination of Benefits
The document below is a brief overview of how plan coverage works when someone has dual coverage.
Taking a Specialty Medication?
You will need to use CVS Specialty® to fill your specialty medications. If you try to fill a medication from the specialty pharmacy drug list (see "Drug Lists & Costs" section below) at your pharmacy of choice, you will be required to submit the prescription to CVS Specialty pharmacy. CVS Specialty provides personalized specialty pharmacist services like:
- A CareTeam who understands your condition.
- Access to a pharmacist and nurse specially trained in your condition. You can call them with questions anytime, any day of the year.
- Help for managing symptoms and side effects.
- Ability to send secure messages from your desktop or mobile phone.
- Option to choose pick up or delivery for your prescriptions. Pick them up at CVS Pharmacy® locations (including those inside Target stores) or have them delivered to your home, work or other place.
- Digital tools available on www.CVSspecialty.com and the CVS Specialty mobile app to help you stay on track with your prescriptions, order refills, get reminders and more.
Taking a Maintenance Medication?
Maintenance Choice® The State uses CVS Caremark's Maintenance Choice program. Under this program, you can save money by obtaining 90-day supplies of maintenance medications (see "Drug Lists & Costs" section below) for the co-pay price of a 60-day fill. This program applies to long-term maintenance medications ONLY and does not apply to short-term/acute medications like antibiotics. Specialty drugs are not available under the Maintenance Choice Program; they are available by mail through the CVS Specialty Pharmacy.
Filling your maintenance prescription After one 30-day fill of a maintenance medication at any participating retail pharmacy, you will receive a letter from CVS Caremark with information on Maintenance Choice and instructions on how to proceed.
- If you fill your maintenance prescription at CVS/pharmacy, a CVS pharmacist can reach out to your doctor to help you obtain a 90-day prescription.
- If you fill your maintenance prescription at a non-CVS/pharmacy, you will need to obtain a 90-day prescription from your doctor unless you opt out of the Maintenance Choice program (see below).
CVS Customer Care or mail order Under Maintenance Choice, you can pick up your 90-day supply at a CVS/pharmacy (including those located inside Target stores) or receive your order at home via CVS Caremark Mail Service Pharmacy.
- For pick-up at a CVS/pharmacy—call your CVS/pharmacy, and they can help you get a 90-day prescription from your doctor, or ask your doctor to send a new 90-day prescription to your CVS/pharmacy.
- For delivery by mail—sign in or register on www.caremark.com to request a new 90-day prescription, or call CVS Customer Care at 800-307-5432 for assistance through the process.
Opt-out for 30-day fills You are not required to use CVS/pharmacy or CVS Caremark Mail Service Pharmacy to fill your maintenance medications. If you want to continue receiving 30-day supplies of your maintenance medications at your preferred non-CVS pharmacy, you can opt out of the program by contacting CVS Customer Care at 800-307-5432. Please note:
- If you continue to receive 30-day fills of your maintenance medications and do not opt out of Maintenance Choice, you will pay the FULL cost for your maintenance prescriptions, not the standard co-pay amounts.
- If you or your dependent(s) contact CVS Caremark to opt out of Maintenance Choice, the opt out will occur at the member level, not the drug level. This allows any eligible covered prescriptions for that member to be dispensed at any participating retail pharmacy without having to call CVS Caremark with every prescription.
AccordantCare for Complex Conditions
If you or a loved one suffer from a complex condition, AccordantCare™ from CVS/Caremark will be able to provide one-on-one support from nurses who are specially trained in complex conditions. It helps you or your covered dependent(s) stay as healthy as possible while living the best life possible. Best of all, this extra support is available on your terms. You can use the program as much or as little as you like. If you’re managing any of these complex conditions, you’re eligible for AccordantCare. It’s part of your Anchor medical plan at no extra cost.
- ALS
- CIDP
- CKD
- Crohn’s Disease
- Cystic Fibrosis
- Dermatomyositis
- Epilepsy
- Gaucher Disease
- Hemophilia
- Hereditary Angioedema
- HIV
- IBM
- JIA
- Multiple Sclerosis
- Myasthenia Gravis
- Parkinson’s Disease
- Polymyositis
- PAH
- Rheumatoid Arthritis
- Scleroderma
- Sickle Cell Disease
- SLE/Lupus
- Ulcerative Colitis
Watch this video, and review the AccordantCare FAQ and AccordantCare flyer for more information. If you have questions or you’re ready to enroll, call AccordantCare at 844-948-0855 Monday – Friday, 8AM – 9PM ET.
Need Help Understanding Your Plan?

Visit the virtual benefits fair and the Decision Support page for tools such as ALEX® and benefits videos & presentations that can help you better understand your plan.
Drug Formularies
A drug formulary is a list of prescription drugs, both generic and brand name, that are preferred by the State's health plan.* CVS Caremark formularies are updated quarterly.
* The State health plan does not cover erectile/sexual dysfunction drugs, allergenic extracts and drugs used for cosmetic purposes, even if they appear in the lists above.
Check Your Prescription Cost
Find out how much your prescription would cost under your health plan via the CVS Caremark Check Drug Cost Tool:
Savings Advisor
Take advantage of Savings Advisor – a tool on Caremark.com that helps you find savings opportunities on the medicine you need:
If you've registered your account on Caremark.com and have enabled member communications, you will get an email from CVS Caremark when they identify a savings opportunity of $10 or more on prescriptions that cost $15 or more per fill.
In your Caremark.com account, you can access a personalized Drug Savings opportunity page that shows any additional savings opportunities like switching to a lower-cost alternative medicine.
See the Savings Advisor flyer for more information.
You are automatically enrolled in prescription coverage when you enroll in one of the State's medical plans. Please see Medical Coverage for more information on eligibility, the enrollment/waiver process, and premium rates.
- CVS Caremark mails ID cards to up to TWO people in your household. CVS Caremark ID cards are separate from your BCBSRI ID card(s).
- You can print extra cards by logging into your account at caremark.com, select Plan & Benefits at the top of the screen, then select Print Member ID Card. You can also order additional cards by calling CVS Caremark customer service at 800-307-5432.
If you haven't already, review the CVS FAQ for answers to common questions about your prescription coverage.
If you have questions regarding your prescription coverage, please contact CVS Caremark:
- Download and register on the CVS Caremark mobile app.
- Register at the CVS Caremark member portal, www.caremark.com.
- Call customer service at 800-307-5432.